2- What STIVARGA studies provide efficacy/safety data for patients with mCRC?
What STIVARGA studies provide efficacy/safety data for patients with mCRC?
Please review CORRECT trial data below before viewing video
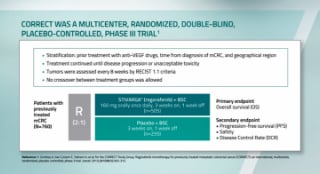
CORRECT trial study design
Multicenter, randomized, double-blind, placebo-controlled, phase 3 trial involving 760 patients1,2
In CORRECT most patient demographics and disease characteristics were similar between arms.
- Patients with previously treated mCRC who had progressed or were intolerant to standard therapies (ECOG performance status 0 or 1)
- STIVARGA: 160 mg orally once daily + BSC 3 weeks on, 1 week off (n=505)
- Placebo + BSC: 3 weeks on, 1 week off (n=255)
- Stratification: Prior treatment with anti-VEGF drugs, time from diagnosis of mCRC, and geographical region2
- Treatment continued until disease progression or unacceptable toxicity2
- Tumors were assessed every 8 weeks by RECIST 1.1 CRITERIA2
- No crossover between treatment groups was allowed2
BSC, best supportive care; ECOG, Eastern Cooperative Oncology Group; RECIST, Response Evaluation Criteria in Solid Tumors; VEGF, vascular endothelial growth factor.
STIVARGA significantly improved overall survival (OS)1,*
- 6.4 months with STIVARGA + BSC (n=505), (95% CI, 5.8-7.3)
- 5.0 months with Placebo + BSC (n=255), (95% CI, 4.4-5.8)
- 23% reduction in risk of death (HR: 0.77 [95% CI, 0.64-0.94] P=0.0102)1
- CORRECT includes patients with historically collected KRAS status (N=729), which was assessed (59% mutant, 41% KRAS wild-type)
- There were 275 deaths out of 505 patients treated with STIVARGA (55%) vs 157 deaths out of 255 patients treated with placebo (62%)1
*OS was the primary endpoint of CORRECT.1
STIVARGA significantly improved progression-free survival (PFS)1,2,†
- 2.0 months with STIVARGA + BSC (n=505), (95% CI, 1.9-2.3)
- 1.7 months with Placebo + BSC (n=255), (95% CI, 1.7-1.8)
- 51% reduction in risk of death or disease progression with STIVARGA [HR: 0.49 (95% CI, 0.42-0.58); P<0.0001]1,2
†PFS, time from randomization to progression or death.2
HR, hazard ratio
Disease control rate (DCR)‡
- DCR included a 41% stable disease rate and a 1% partial response rate in the STIVARGA arm (n=207/505) vs a 15% stable disease rate and a 0.4% partial response rate in the placebo arm (n=38/255)1
‡Disease Control is defined as proportion of patients with a best response of complete or partial response or stable disease; assessment of stable disease had to be made at least 6 weeks after randomization.
Safety profile in CORRECT


§Adverse reactions graded according to National Cancer Institute Common Terminology for Adverse Events version 3.0 (NCI CTCAE v3.0).
¶The term “rash” represents reports of events of drug eruption, rash, erythematous rash, generalized rash, macular rash, maculopapular rash, papular rash, and pruritic rash.
||Fatal outcomes observed.
AE, adverse event; CORRECT, COloRectal cancer treated with REgorafenib or plaCebo after failure of standard Therapy; HFSR, hand-foot skin reaction; mCRC, metastatic colorectal cancer; PPES, palmar-plantar erythrodysesthesia syndrome.
Toxicity-related discontinuation
- Skin toxicity (HFSR/PPE or rash) was the most common cause of permanent drug discontinuation1
- 8.2% of STIVARGA patients discontinued treatment because of drug-related AEs vs 1.2% of placebo patients1
References:
1. STIVARGA. Prescribing Information. Whippany NJ: Bayer HealthCare Pharmaceuticals Inc; December 2020. 2. Grothy A, Van Cutsem E, Sobrero A, et al; CORRECT Study Group. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303-312.
© 2023 Bayer. All rights reserved.
Bayer, the Bayer Cross, STIVARGA and Access Services by Bayer are registered trademarks of Bayer.
Medical Oncologist
Washington, DC